Dr. Jonathan Iralu and Dr. Alithea Gabrellas, two infectious disease specialists at Gallup Indian Medical Center in northwestern New Mexico, believe in the power of the ECHO Model to transform HIV care.
“We have almost 100% of our patients on antiretroviral therapy, and we achieve virologic suppression in about 90% of the patients. Seeing that kind of improvement over decades is really, really good. I think ECHO is largely responsible for those improvements,” says Dr. Iralu, who has been leading the Indian Country HIV ECHO for a decade.
In 2003, when Dr. Iralu first started treating HIV at a clinic in Gallup, New Mexico, a team of Indian Health Services doctors would have periodic phone calls to discuss their cases—but, it didn’t have much structure. When they saw the success of Project ECHO’s Hepatitis C Program, they realized its model could also work for their HIV patients. The ECHO Model, inspired by the way clinicians learn from medical rounds during residencies, provides a virtual community where participants share support, guidance and feedback on cases.
An Answer that Echoes
In 2009, Dr. Iralu looked for an ECHO program to improve his knowledge and capacity for treating HIV; and he discovered the ECHO program created by the New Mexico South Central AIDS Education and Training Center, part of the federal government’s network of HIV experts providing cost-free, locally-based targeted education. By 2013, there were enough providers joining to create an ECHO program specifically geared to those serving Indian Country, or the lands and communities where Native people live.
“In terms of patient care, I don’t see how we could possibly treat this many people for HIV without having this ECHO in place,” Dr. Iralu says. “Our participants call us between ECHO sessions and say things like, ‘Hey, that patient we discussed last week broke out in a rash from that drug you recommended,’ for instance. ECHO provides a forum where we can work through questions and teach people on the fly.” The Indian Country HIV ECHO program started in northwest New Mexico, quickly spread to Arizona, and today, participants join from all over the Southwest.
A System-Level Impact for Rural Providers
“ECHO has an incredible multiplying effect,” Dr. Gabrellas adds. Unlike the silos that take place in the clinic setting, participants joining the HIV ECHO include all aspects of wraparound services: specialists, case managers, social workers and peer support teams.
A single ECHO session can include broad range of participants, ranging from a rural nurse practitioner with her first HIV-positive patient, to a board-certified infectious disease doctor with a complicated case. “People can bring any type of HIV case to the ECHO, and get feedback and support,” she says.
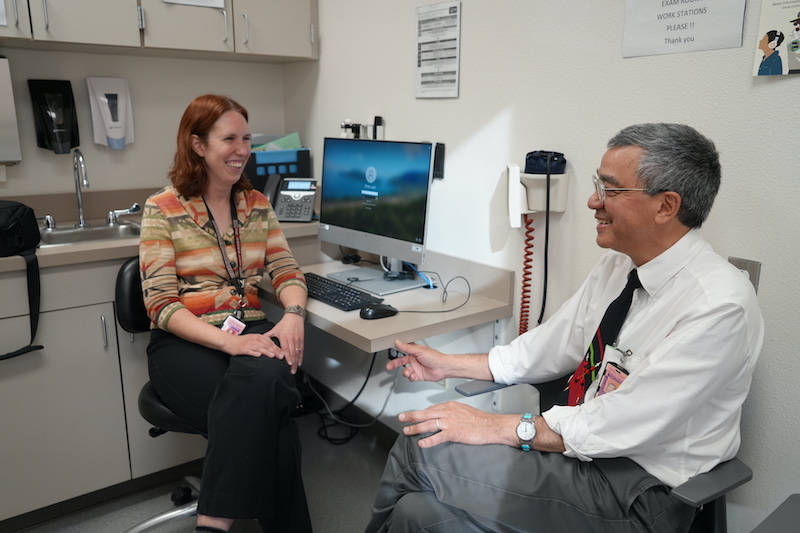
Dr. Gabrellas, left, and Dr. Iralu now work together to support patients in the Indian Health Services system after meeting through Project ECHO. Photo Credit: Sarah Helms for Project ECHO, January 2024.
Amplifying Physician Capacity in New Mexico and Across the Country
They now have participants from rural and urban locations all over the country. “With ECHO’s telementoring, a primary care provider at a rural clinic becomes a resource for the other providers and other staff of that clinic as well,” Dr. Gabrellas adds. “It’s great for a rural system like the Indian Health Service, which doesn’t have a lot of specialists. These frontline primary care providers in a lot of rural, small clinics can have access to real mentoring with ECHO.”

Gallup, New Mexico, where the Indian Country HIV ECHO started, is a town of nearly 22,000 people bordered by the Navajo Reservation. Photo Credit: VisitGallup.com
A Long-Term Provider Support Network
The ECHO Model also creates a long-term network of support for providers in times of crises and burnout. During the pandemic, the HIV ECHO program expanded to sessions on HIV care-provider wellness, offering a safe space to discuss loss and isolation to nurses, technicians, pharmacists, and doctors.
“ECHO makes it feel like it’s not you alone providing the care for HIV in a rural area, it’s that entire team [of providers],” Dr. Gabrellas explains. “Then, over time, your confidence and expertise grow.”
Speaking to 10 years of groundbreaking gains in HIV/AIDS care, SCAETC Program Director Tracy Jungwirth says, “We, at the SCAETC, and especially our local partner site at The University of New Mexico, are honored to work with Dr. Iralu and his team. We know this collaboration impacts health care team confidence in HIV care, and the result has been an increase in HIV viral suppression and in HIV pre-exposure prophylaxis use, decreasing the rates of new HIV infection and ultimately resulting in improved health outcomes.”
Acknowledgement:
The Indian Country HIV ECHO Program is made possible through funding from the U.S. Health Resources and Services Administration and is implemented as a part of the South Central Aids Education Training Center’s Education and Training mission.
Learn more
Support Project ECHO’s work or participate in the free Indian Country ECHO programs, visit our webpage at iECHO.org.
*Featured Image: Dr. Iralu at the Gallup Indian Medical Center. Photo Credit: Sarah Helms for Project ECHO, January 2024.


