According to The Lancet, bacterial antimicrobial resistance caused 1.27 million deaths in 2019 and played a role in about 5 million deaths worldwide.
Often caused by over-prescribing and lack of access to the right antibiotics, health care providers are seeing pathogens with increased resistance to antimicrobials, which makes common infections—including bloodstream infections, pneumonia and tuberculosis—much harder to treat. The results can be devastating: from higher medical costs and less effective antimicrobial treatments, to prolonged illness and more unnecessary deaths.
“The challenges around antimicrobial stewardship are complex and we need a multisectoral approach with industry, government, and nongovernmental partners to drive real impact. With an estimated average drug resistance rate of 76%, this crisis calls for targeted interventions,” says Elif Aral, Pfizer’s Access and Accord Commercial Lead for Emerging Markets.
A Systems-Level Intervention: TEACH AMS
To support this global effort, Project ECHO and Pfizer partnered to launch the Telementoring, Equity and Advocacy Collaboration for Health through Antimicrobial Stewardship ECHO Program, or TEACH AMS, in 2023.
This initiative uses the ECHO Model to teach and mentor frontline health care workers in the Global South. The sessions provide guidance and support between peers and subject matter experts to foster virtual communities of practice and implement antimicrobial stewardship (AMS) programs in hospitals to ensure access to best-practice care for patients across Africa and Latin America.
“Each case [presented during an ECHO session] brings new ideas, so you are able to learn and borrow from those [hospital] sites. Each site shares a unique challenge and how they tackled it. It is a whole package on how you manage a patient from clinical, diagnostic and pharmaceutical perspectives,” says Dennis Ndeto, laboratory officer, at the Machakos Level 5 Hospital in Kenya.
By building the capacity of local, regional, and national stakeholders, the TEACH AMS initiative supports the implementation of sustainable AMS programs in hospitals and health care facilities to minimize the harmful consequences of antimicrobial misuse and bacterial antimicrobial resistance.
Participants learn about appropriate antimicrobial prescribing practices and establish systems for monitoring antibiotic prescribing and use. These active AMS practices ensure patients receive the correct anti-infective treatments for the right duration and according to evidence-based guidelines.
In Africa, Immediate Impact with Sustainable Results
With seven programs in Africa and a regional program in Latin America, TEACH AMS has reached more than 3,000 health care providers in 78 countries. Laboratory personnel, microbiologists, nurses, pharmacists, physicians, pharmacy technicians, and others have attended the 131 sessions, logging more than 14,000 total attendances since the initiative began in January 2023.
TEACH AMS participants are implementing new skills, resulting in tangible practice and system changes and improved workplace practices. In a survey, nearly all participants (91%) said they intended to—or were already—integrating the knowledge they gained from the TEACH AMS ECHO programs in their professional practice. Participating facilities report working as an integrated team with a multidisciplinary approach to patient management.
“The lessons learned from ECHO have guided us in diagnostic stewardship: how to carry out tests in the lab, report test outcomes, and the select appropriate antibiotics for each case,” says Dr. Marian Nyamokami Ongayo, clinical pharmacist at the Mbagathi Level 5 Hospital in Kenya.
Providers are seeing better patient outcomes — along with an improved pattern of antibiotic prescribing—as health care facilities begin using data to monitor antibiotic prescriptions and outcomes.
“We’ve been able to improve how we manage cesarean sections by preventing infections. Through the ECHO sessions, we are able to learn about antibiotic prophylaxis [using antibiotics to prevent infection rather than treat them] and start using recommended antibiotics. We’re tracking cesarean section infection rates in the labor ward, and we found that cases are going down because of increased knowledge in infection prevention,” says Lucy Beatrice Mwai, Infection Prevention and Control nurse at the Thika Level 5 Hospital in Kenya.
WATCH: TEACH AMS ECHO Participants Discuss the Program’s Impact
Taking the Fight to Latin America
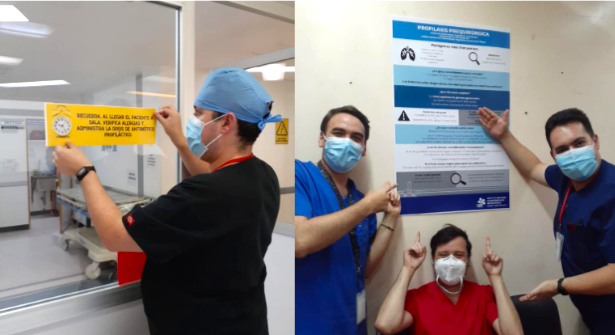
The team at the National Institute of Respiratory Illnesses (Mexico City, Mexico) promotes the rational use of antimicrobials and its impact on the use of antimicrobial pre-surgical prophylaxis. They are part of the TEACH AMS ECHO Program. Photo Credit: Not Known
Since 2023, TEACH AMS has started ECHO Programs in Ghana, Kenya, Malawi, Rwanda, Senegal, Uganda and Zambia. In March 2024, they launched the TEACH PROA ECHO Program in Latin America.
Spearheaded by PROAnet, a nonprofit based in Argentina, the TEACH PROA ECHO Program noted a significant shift in health care practices and antimicrobial stewardship across participating facilities. Microbiologists, pharmacists, physicians and physician assistants participate from private and non-profit institutions.
Collaborating with 139 health care facilities in 13 countries, PROAnet also provides tools to improve antimicrobial use and combat resistance, including a web platform and a mobile app in Spanish with dosing and clinical guidelines – tools used by more than 17,000 professionals.
In a follow-up survey, PROA ECHO participants reported making positive changes in their practices by adapting or creating clinical guidelines within their facilities; increasing frequency of taking cultures; ongoing learning from colleagues; and reducing daily doses of antibiotics. By promoting a culture of continuous improvement, participants are empowered to turn what they have learned into lasting changes in their practice.
Education and Mentorship are Our Best Tools
As TEACH AMS enters its third year, the TEACH AMS programs in Africa will grow, with participating countries Ghana and Malawi cascading their programs to a sub-national level. In Latin America, the PROA team plans to launch “Project IMPROVE” to focus on quality improvement of antimicrobial practices throughout 22 public and private health care facilities in 10 countries.
“Data from the program’s monitoring and evaluation efforts show evidence of the significant impact of TEACH AMS programs. Participants report applying the knowledge gained in the sessions and adopting best practices, and note patient improvements. There have also been documented improvements in the core facility AMS capacity elements needed to build sustainable AMS programs,” says Amy Groom, executive project director.
Antimicrobial resistance is not an intractable problem. With targeted training and ongoing mentorship, health care facilities and providers in even the most underserved communities can implement robust AMS programs.
WATCH: TEACH AMS ECHO participants discuss the program’s impact
Learn more about Project ECHO’s antimicrobial stewardship programs.
Featured Image: Participants from the National HIV Reference Laboratory virtually joining the ECHO TEACH AMS Senegal launch event. From left to right: Professor Halimatou Diop-Ndiaye; Professor Cheikh Saad Bouh Boye; Professor Awa Ba Diallo; Professor Seynabou Lo. Credit: Alphonse Konan Assouman, Project ECHO, October 2024

