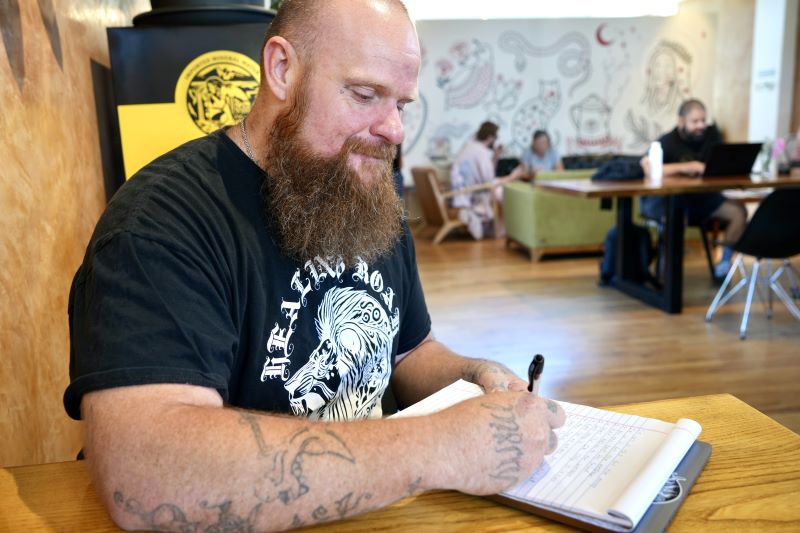
Matthew Pettit, a certified peer support worker, has worked with Project ECHO since the beginning of his recovery journey from a decades-long addiction to methamphetamines.
In New Mexico’s Community Health Worker and Peer Support Worker Opioid ECHO Program, he found an outlet to support other people on their personal – and professional – paths. Below, Pettit shares his story through a first-person narrative.
“I’m here to say that ECHO makes a difference,” says Pettit, a peer support worker who lives in Albuquerque, NM. For nearly three years – first as a participant, now as a facilitator – Pettit has been part of the CHW/PSW Opioid ECHO program, offering 12 weeks of training and networking to new workers. Pettit and his colleagues primarily work with clients in need of support with substance use and opioid use disorders.
“Any time I have an opportunity to use my experience, it helps me heal and continue to move forward, too.”

Matthew Pettit, a certified peer support worker, sees the Project ECHO community as part of his personal journey in recovery. Photo Credit: Sarah Helms, Project ECHO, April 2024.
Finding Tools to Heal, with ECHO
“I spent 20 years of my life without the tools I needed to heal. The very first time I attended an ECHO session, I loved it. It was the fact of the ECHO Model itself, where people with lived experience can share their knowledge.”
In an ECHO program, experts provide short lectures and participants present client cases; as a group, they troubleshoot challenges and brainstorm solutions — a critical component of ECHO’s “all teach and all learn” model.
For the CHW/PSW Opioid ECHO, experts share best-practices in trauma-informed care, opioids and pregnancy, and how to support friends and family. “There’s lived experience and learned experience, and we need both. ECHO allows people to come and share, learn, and be around like-minded individuals with similar lived experiences and share with experts. ECHO helps the entire community because the healthier the peer support worker, the more help we can offer our clients.”
“Research shows that 30% of a client or patient’s recovery outcome depends on the relationship between the client and the provider. It’s a lot easier for individuals to connect with someone who has lived experience – someone who’s been through the same thing they are going through.”
“A probation officer can say something to a client and the client feels attacked and un-supported. I can say the exact same thing, and get an entirely different response. The client knows I’m on their side and have been through the same thing. When I speak, they hear,” says Pettit, who is currently earning his associate’s degree. “I wouldn’t trade a year of my lived experience—20 years of my life on what we call ‘hard’ drugs—for anything I’ve learned in school.”
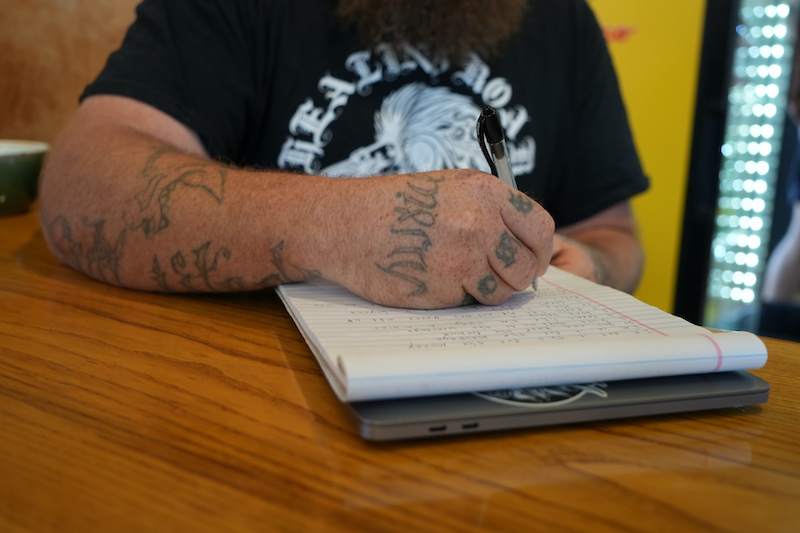
Pettit uses writing, stand-up comedy, and advocacy as outlets to have honest conversations about recovery from substance use and opioid use disorders. Photo Credit: Sarah Helms, Project ECHO, April 2024.
A Community Network for Better Care
The program provides professional connections for participants. This is critical because “the best peer support workers are the ones with the best networks,” says Pettit.
Resources—housing vouchers, prescriptions, long-term therapies—can be hard for an individual peer support worker to find. Being able to leverage an entire network ensures clients get faster, better solutions and their support workers face less professional stress.
“I had one client who was unable to get medication [methadone] after he moved to New Mexico from out of state. There was a high probability that he’d find another form of pain relief; and here [in Albuquerque] that’s most likely to be fentanyl. Only by presenting this case [in an ECHO session] did I find out that there were a couple of places that would be able to prescribe him methadone as an ongoing medication. For my client, that is life-saving.”
“ECHO makes sure we all get the support we need, and that our clients have the support that they deserve. It’s public health work, but it’s always because of that personal connection. ECHO makes space for that,” says Pettit.
To learn more about the New Mexico CHW/PSW Opioid ECHO Program or to reach out to the program team, visit the iECHO page.