When José “Joe” Rivas, a medical case manager at First Nations Community HealthSource, a federally qualified health center, talks about the impact of Project ECHO’s Opioid Crisis and Pain Management program, he’s not just speaking as a health care professional; he’s speaking from lived experience.
Joe Rivas takes part in the Opioid Crisis and Pain Management ECHO program from his office in Farmington, NM. Credit: Theresa Graven, Project ECHO, February 2025.
For years, Joe lived in a fog—physically and mentally—after a botched dental procedure left him with trigeminal neuralgia, a nerve condition that can cause severe, debilitating pain. Chronic pain led him down a well-worn path: one that begins with a doctor’s prescription but often ends in a vicious cycle.
As a medical case manager, Joe witnessed the stigma, frustration and barriers people face when trying to recover from substance use, especially in New Mexico’s rural and tribal communities—challenges that make pain management even more complex.
“I was on opioids for years, and they did nothing but dull me. It became impossible to function at my best. I wasn’t fully present for my clients, and my personal life was unraveling, too.”
Joe’s turning point came when his primary care provider suggested buprenorphine, a medication commonly used for opioid use disorder that is increasingly recognized for chronic pain management.
By combining buprenorphine with mindfulness and meditation, and finding a provider who truly understood chronic pain, Joe found his way out of opioid dependence.
“Once I emerged from that fog, I realized how many of my clients were still stuck in it: facing the same stigma and isolation I had experienced,” he says.
Seeking tools to support his clients, Joe turned to Project ECHO.
Expanding ECHO’s Impact Across New Mexico
Joe works in Farmington, a rural community bordering the Navajo Nation, where health care access is limited, transportation is a challenge, and provider shortages make consistent care difficult. Many of his clients struggle with chronic pain, substance use disorders, and the lasting effects of historical and systemic trauma.

Shiprock, also known as Tsé Bitʼaʼí (Winged Rock), on the Navajo Reservation in San Juan County, New Mexico. Credit: Julie Francois, Flickr – used with permission
Joe helps coordinate care—including testing, treatment and referrals—for people living with hepatitis C, HIV and sexually transmitted diseases.
Joe also plays a key role in “harm reduction” in his community, offering practical strategies to the negative consequences of drug use. Joe distributes naloxone, the opioid-overdose antidote; connects patients with syringe exchange programs and counseling services; and, generally, provides education on overdose prevention.
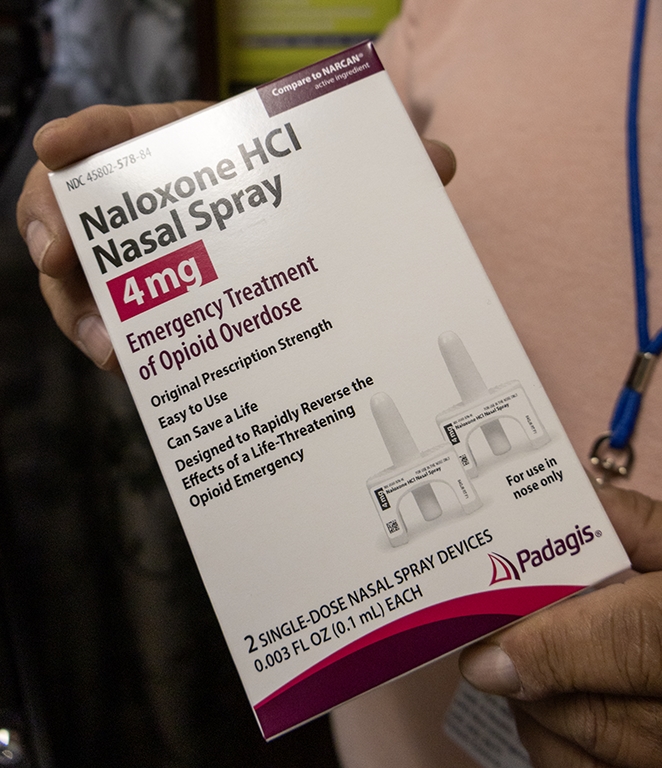
Naloxone, an opioid overdose reversal medication, is helping to save lives and support harm reduction in rural New Mexico. Credit: Theresa Graven, Project ECHO, February 2025.
“When I saw the description of the ECHO sessions, I thought: ‘This pertains to me. This is my lived experience,’” says Joe. “I was reminded of the most fundamental skill in medicine: listening, really listening, to where someone has been, where they are, and where they hope to be.”
Project ECHO deepened Joe’s expertise in pain management and harm reduction, offering practical strategies to non-opioid pain management; trauma-informed care; and approaches to reducing stigma. Through the ECHO Model, Joe has the opportunity to present cases and receive collaborative feedback from a team of specialists, including behavioral health experts, physicians and psychologists.
Patient-Centered Care in Underserved Communities
One of Joe’s most memorable clients was a man who had lost his teeth—a visible marker of addiction’s toll. When the client first arrived at the harm reduction clinic, he was hesitant and ashamed, barely making eye contact. Like many in rural areas, he had been dismissed or ignored by the health care system, struggling to access even basic care.
“In these communities, stigma around substance use runs deep. Many people I work with feel like they don’t deserve medical care. They hear it from family, friends, even from health care providers who refuse to prescribe medication or from pharmacies that won’t provide syringes. They internalize it until they believe they are unworthy of help,” says Joe.
Joe applied what he learned from ECHO:
- Meet the individual where they are — without judgment
- Help them see they are worthy of care
- Provide harm reduction services with compassion
“We didn’t push him. We listened. We reassured him that he deserved care; that his struggles did not define his worth.” Weeks passed. When the man returned to the clinic, he had a brand-new set of dentures—and a big smile.
“That moment solidified what I had learned in ECHO. It’s not just about treatment plans—it’s about changing the way our clients see themselves. Helping them shift from believing they’re undeserving to knowing they are worth fighting for.”
The Lasting Impact of Project ECHO
For Joe, Project ECHO has been more than just professional development, it has been a lifeline.
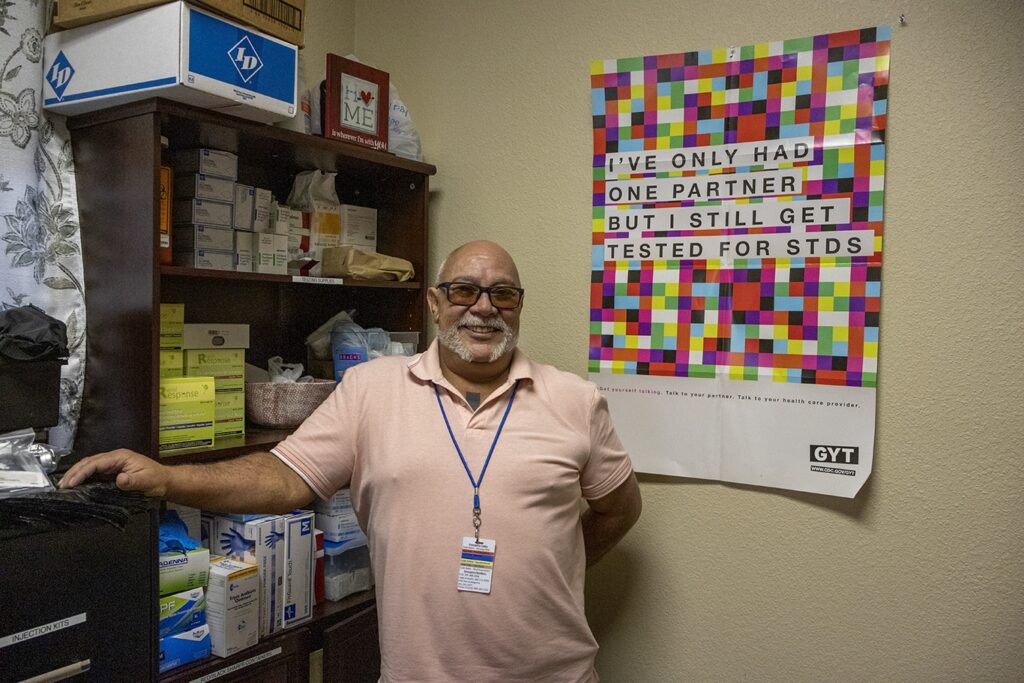
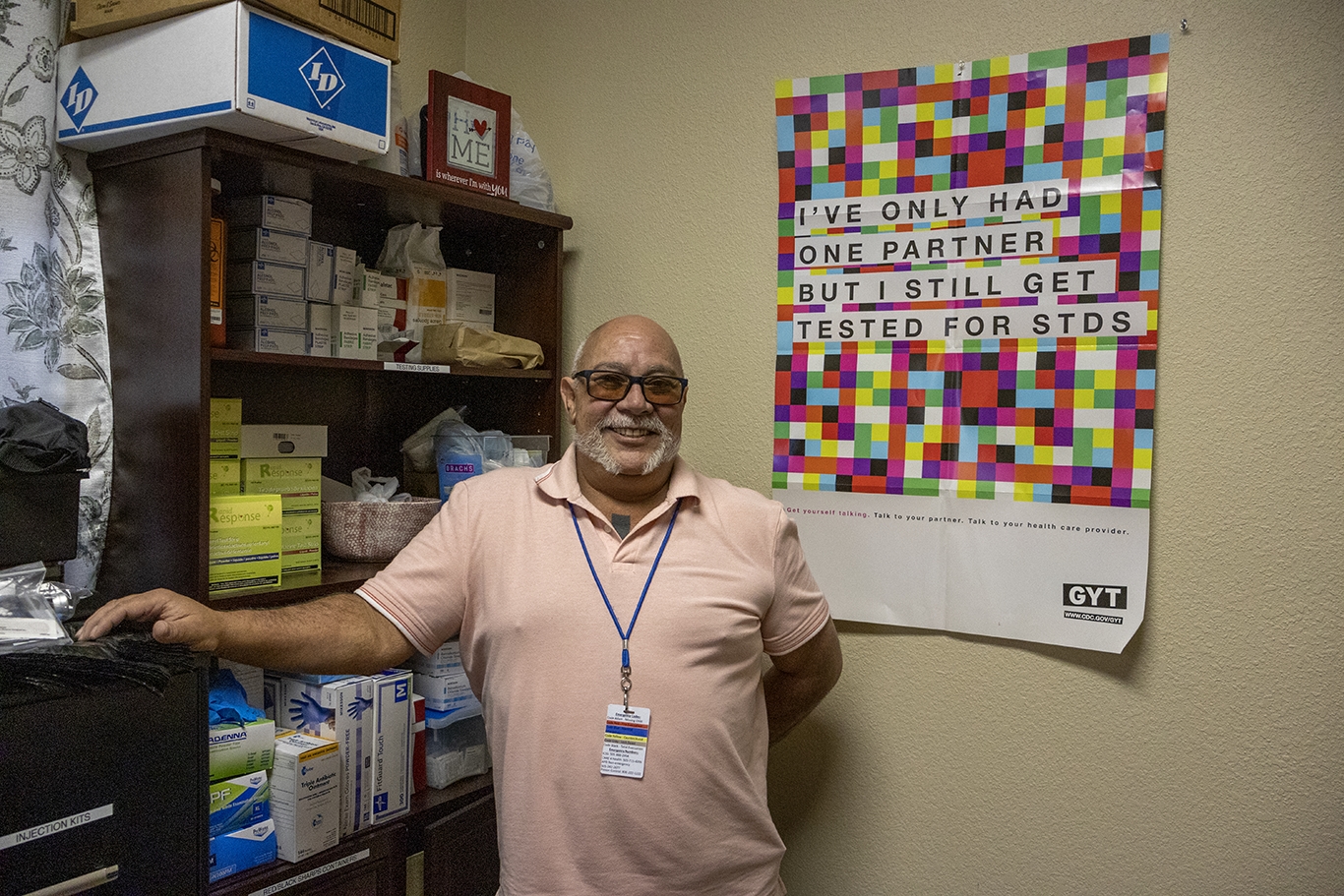
Joe Rivas stands in front of harm reduction and STI testing supplies. Photo Credit: Theresa Graven, Project ECHO, February 2025.
“These sessions remind me that I’m not alone in this work. They connect me to providers who are committed to humanizing medicine and breaking the cycle of stigma. Every time I sit in on a session, I leave with new strategies, renewed confidence, and a stronger ability to have difficult conversations with my clients, helping them see a future beyond opioids.”
By bringing ECHO’s knowledge directly to the frontlines, Joe is helping bridge the health care gap for New Mexico’s most at-risk communities, so the people who need care the most are no longer left behind.
To learn more about the no-cost Opioid Crisis and Pain Management ECHO Program, register on iECHO.org, Project ECHO’s telementoring platform.
Join experts and participants in ECHO’s “all learn, all-teach” model, spearheaded by Dr. Joanna Katzman, who has been instrumental in expanding access to evidence-based care for chronic pain and opioid use disorder across New Mexico and nationally.
Featured Image Credit: Joe Rivas stands in front of harm reduction and STI testing supplies. Credit: Theresa Graven, Project ECHO, February 2025.
Originally published in February 2025, this story was re-published in January 2026 to add credit to the authors.